Wednesday, October 29, 2003
3643
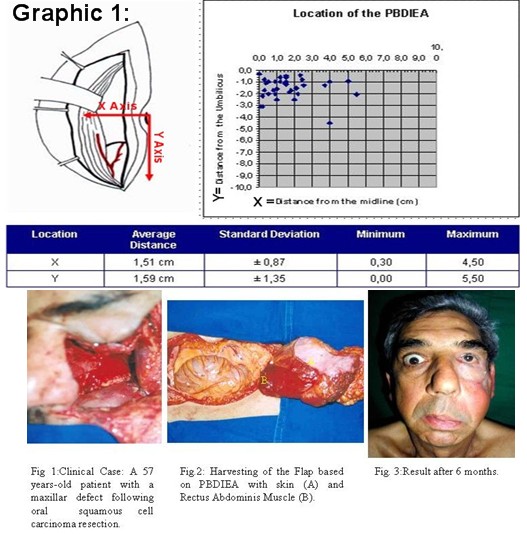
P25: Anatomical Analysis of Fascioperitoneal Flap Based on the Peritoneal Branch of the Deep Inferior Epigastric Artery (DIEA)
Peritoneum has great capacity of squamous metaplasia and is resistant to gastric secretions and radiation exposure. In 1990 Mixter described the use of a composed fascioperitoneal flap based on the peritoneal branch of the deep inferior epigastric artery (PBDIEA) in five patients for intraoral reconstruction. An anatomical study in 17 fresh cadavers (less than 24 hours of death) with average age 62.3±13.49 years and mean weight 63.5± 9.47 kg was done totalizing 34 anatomical regions with the objective to establish anatomic parameters of this flap and the vascular territory of the PBDIEA. A histomorphometric study of the vessels was also done. Cadavers with previous abdominal surgery were excluded. In order to determine anatomy of the vessels and the PBDIEA vascular territory , the DIEA was cannulated with an 18-gauge catheter and injected with blue ink latex. A square-lined map of 1x1 cm was used for standardization.The following parameters were measured: location, distribution and distance from the midline and umbilicus. Anatomy and distribution of the PBDIEA was observed in the lower abdomen. (Graphic 1) The vessels were then resected and fixed in 10% buffered formalin and 70% alcohol, embedded in paraffin and 5 mm perpendicular sections were cut and stained with hematoxylin and eosin. A digital camera and light microscopy (Zeiss Axioplan tm) were used to capture the specimen’s image. These images were morphometrically evaluated using computer-aided image analysis software (Oculus TCX / Optimas v.4.10 tm) Results: In all cadavers were found PBDIEA bilaterally. In three cadavers there was also an accessory branch of the deep inferior epigastric artery to the peritoneum. The average PBDIEA length was 3.55 ± 1.33 cm. Total length until the origin of deep inferior epigastric artery: 9.38 ± 3.31 cm. Average external diameter: 0.304 ± 0.074 mm. The PBDIEA vascular territory has an average size of 10.9 x 7.13 cm. Conclusion: The peritoneal branch of the DIEA has one constant vascular pedicle, with relatively permanent anatomical localization and a good arc of rotation.This flap can be dissected together with the rectus abdominis muscle or associated with skin.(Fig 1-3) Due to the small diameter of the PBDIEA the microsurgical anastomosis is very difficult, however the deep inferior epigastric vessels can be transferred with this flap.
View Synopsis (.doc format, 108.0 kb)
See more of Posters
Back to Plastic Surgery 2003 Complete Scientific Program
Back to Plastic Surgery 2003 Meeting home