Wednesday, October 29, 2003
3628
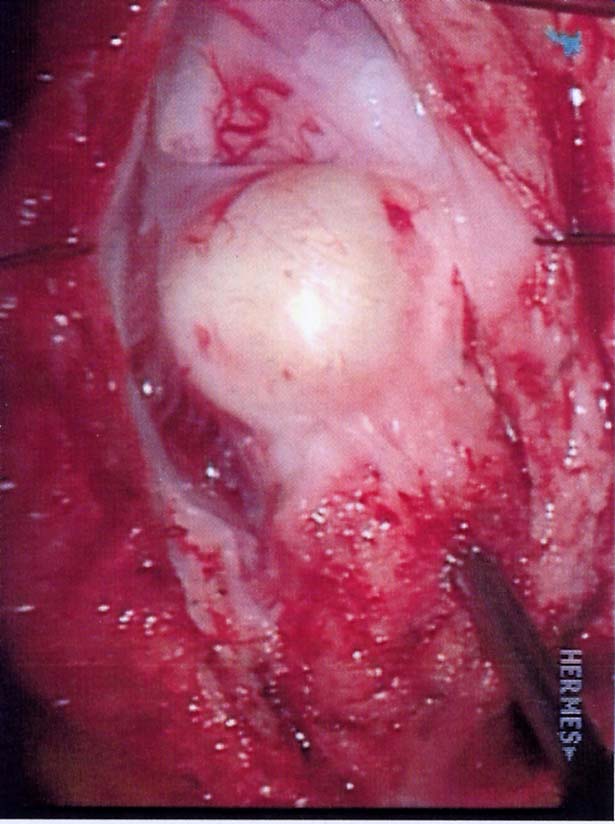
P52: Intraspinal Epidermal Cyst Following Intrauterine Surgery as Cause of Difficult to Heal Myelomeningocele Repair
Intraspinal epidermal cysts are unusual, accounting for less than 1% of all spinal tumors. These benign tumors are thought to arise from aberrant ectodermal rests during embryogenesis or the iatrogenic implantation of cutaneous elements during instrumentation of the spinal canal. Prior to the introduction of the styleted spinal needle, up to 40% of reported cases were attributable to previous lumbar puncture. With advances in prenatal diagnosis and technical improvements in the field of neurosurgery, postconception repair of the myelomeningocele is now commonplace. Consequently, the intraspinal epidermoid cyst is a rare but documented sequela. These cysts may continue to slowly enlarge and may not become symptomatic for up to fifteen years. In addition, the associated surrounding inflammation can contribute to retethering of the cord. The authors report a case of a patient diagnosed with a neural tube defect prenatally. The patient underwent intrauterine repair for closure of the defect and was born at 34 weeks gestation. The child developed a wound breakdown following release of a tethered cord at three months of age. Despite multiple attempts at fasciocutaneous coverage, muscular coverage, and full thickness skin grafting using the patient's foreskin, there was persistent drainage from the wound and a delay in healing. Exploration for a retethered cord revealed a posteriorly positioned intraspinal epidermal inclusion cyst with surrounding inflammation, granulation, and tethering. After removal of the cyst and turnover paraspinal muscle flaps, the patient has healed uneventfully. With the continued emergence of intrauterine myelomeningocele repair and the sometimes prolonged (up to fifteen years) presentation of the intradural epidermoid cyst, this diagnosis must be entertained in the difficult to heal myelomeningocele reconstruction.
View Synopsis (.doc format, 22.0 kb)
See more of Posters
Back to Plastic Surgery 2003 Complete Scientific Program
Back to Plastic Surgery 2003 Meeting home