Tuesday, October 28, 2003 - 4:00 PM
3469
The Anatomic Basis for the Tear Trough and Crescent Deformity at the Lower Eyelid - Cheek Junction
Purpose: The clinical manifestations of eyelid deformities are extremely variable and tend to be genetically mediated. The tear trough and crescent deformities are pervasive complaints amongst patients seeking to improve the appearance of their lower eyelid region. The arcus marginalis, defined as the confluence of the orbital septum and periosteum, has been determined to be a key component in this deformity pattern. The purpose of our study is to examine the position of the arcus marginalis and measure its relationship with the infraorbital rim through cadaver dissections. Our goal is to come to a more precise understanding of how the arcus marginalis position can bring about these deformities at the lower eyelid – cheek junction. Ultimately, we aim to enhance the efficacy of arcus marginalis release with lower lid blepharoplasty and facial rejuvination surgery in each individual patient.
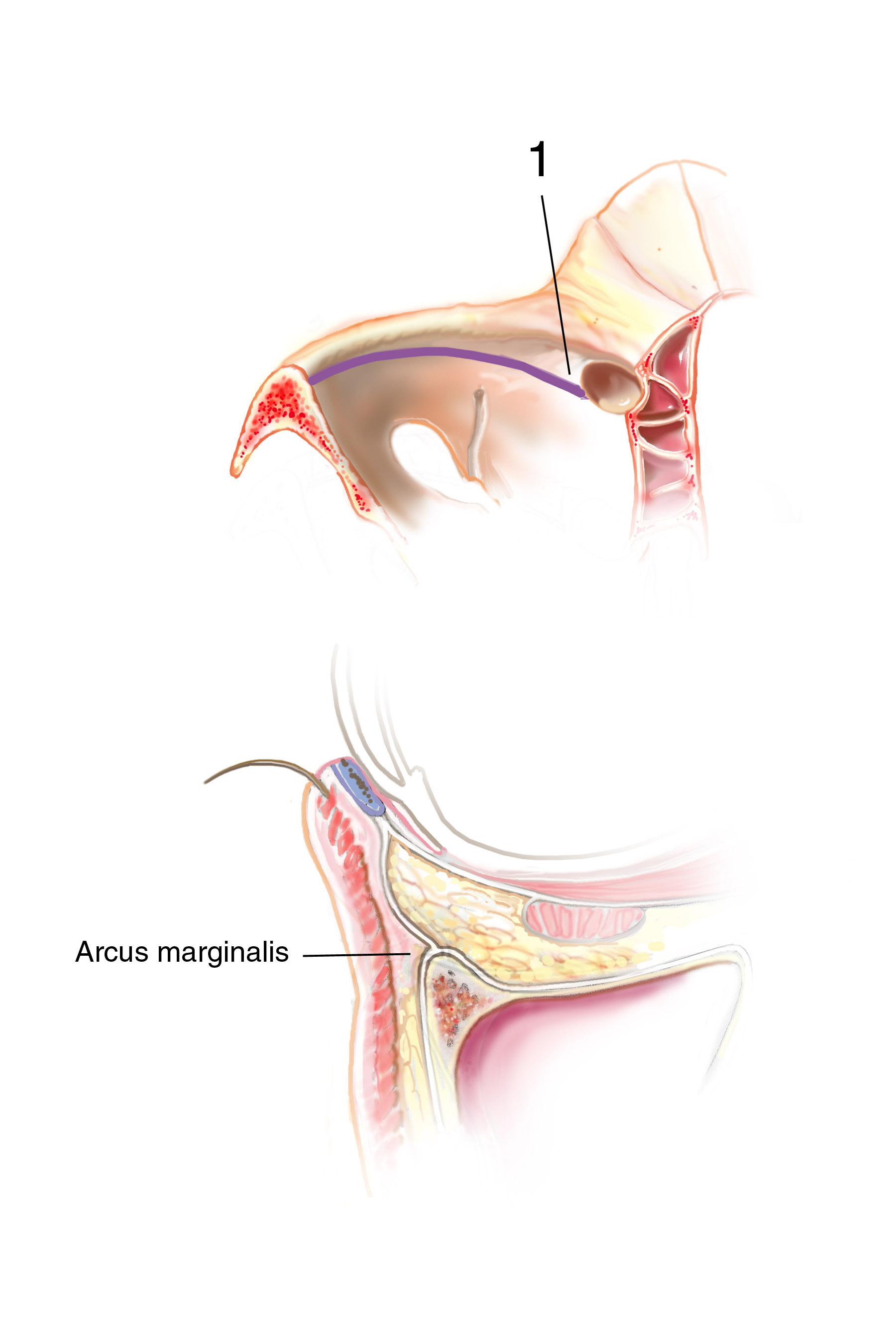
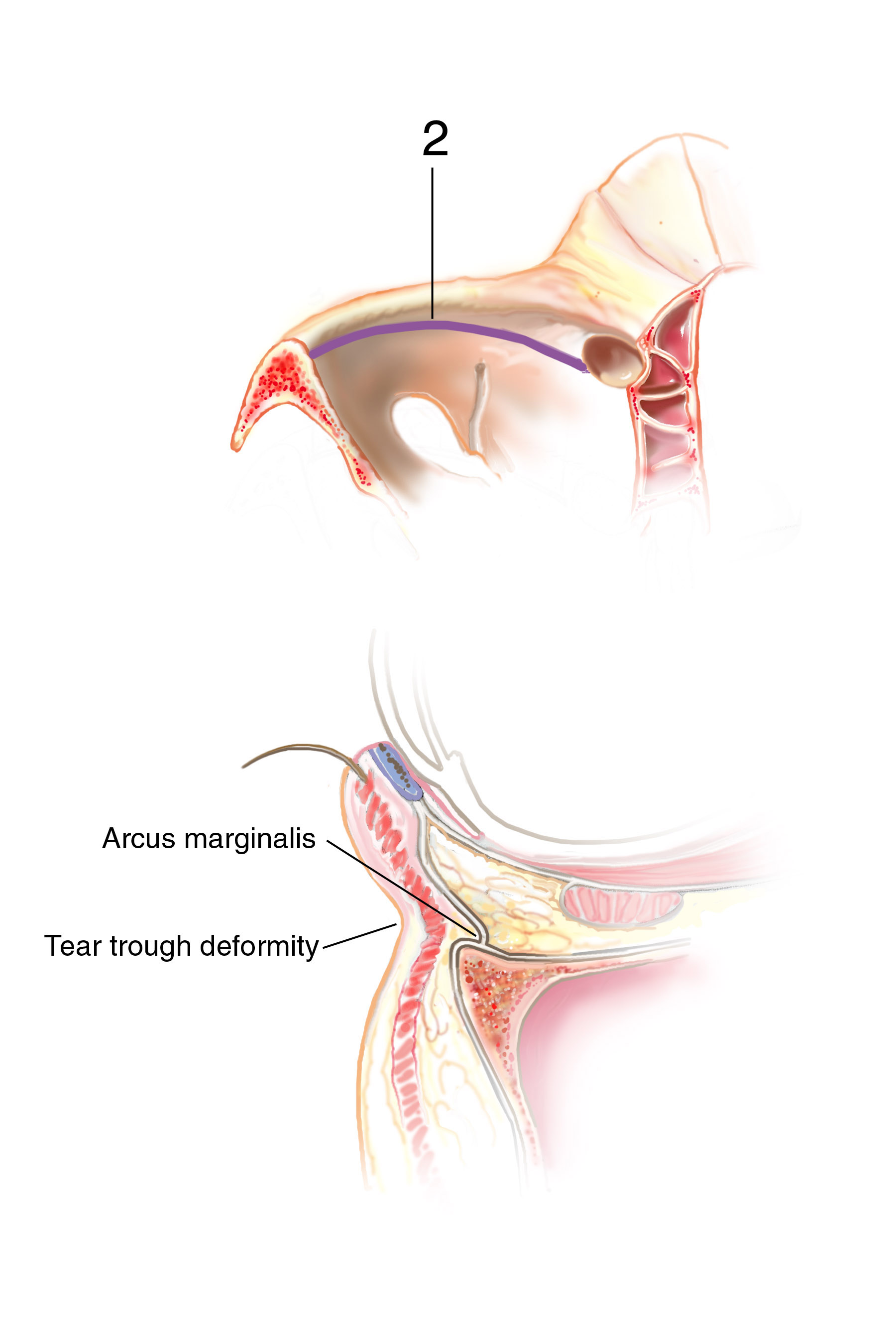
Methods: Dissection of the eyelid and cheek region with analysis of the orbital septum and arcus marginalis position was carried out on 17 caucasian cadavers obtained from the Brown Medical School anatomy course (Figure 1a,b). Of these cadavers, 22 periorbital regions could be accurately measured, 13 from male cadavers and 9 from females. Measurements of the orbital septal attachment into the orbital floor were taken at 5mm intervals starting from the medial canthus and continuing laterally along the infraorbital rim to the lateral canthus. Two measurements were taken at each interval, the first being the anterior-posterior distance from the arcus marginalis to the superior apex of the infraorbital rim, and the second being the distance form the arcus marginalis to the most anterior extent of the infraorbital rim.
Results: In both male and female cadavers, the orbital septum was found to insert posterior to the superior most point of the infraorbital rim. The distance between the arcus marginalis and the infraorbital rim varied from medial to lateral. In male cadavers, the distance between the arcus marginalis and the superior apex of the infraorbital rim measured 4.8mm (3-6) medially to 1mm (1.0mm) laterally. The distance to the most anterior point of the infraorbital rim measured 8mm (6-9) medially to 1.8mm (1-4mm) laterally. In the female cadavers, the distance between the arcus marginalis and the superior infraorbital rim measured 2.9mm (1-5mm) medially to 1mm (1mm) laterally. The distance to the most anterior point measured 5.7mm (4-7mm) medially to 1.3 mm (1-2mm) laterally.
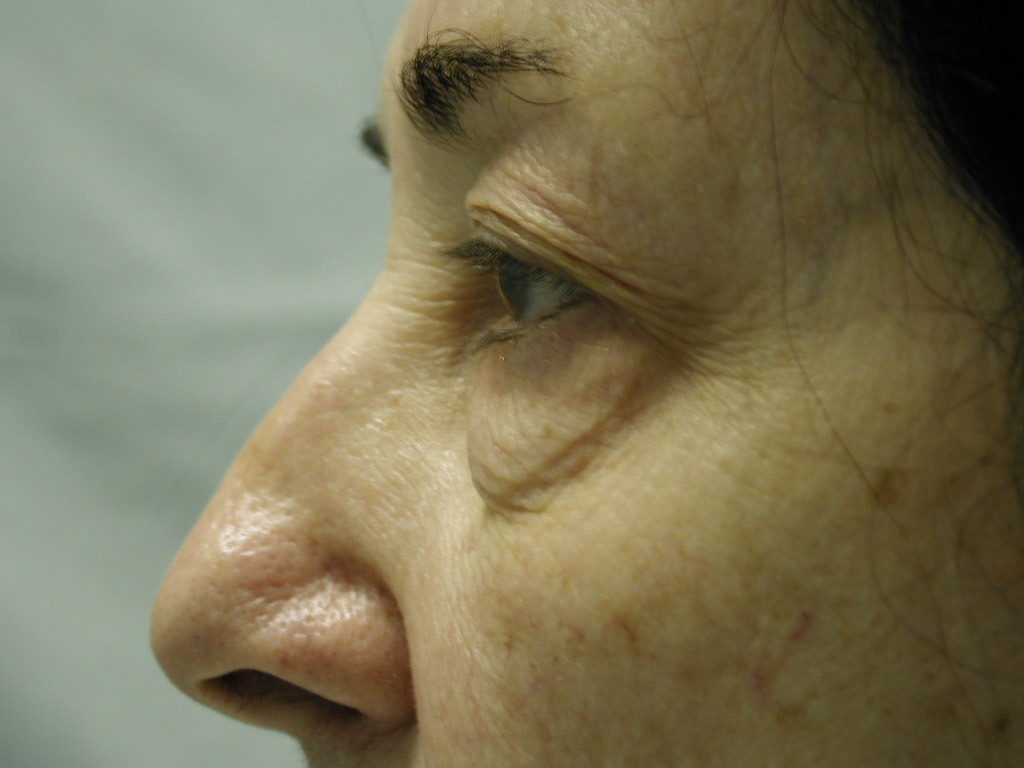
Discussion: Our goal is to determine the anatomic basis for the tear trough and crescent deformities so to optimally blend the lower lid cheek junction in each individual patient. From cadaveric dissections, we have come to three conclusions: First, medially the arcus marginalis attaches posterior to the actual orbital rim as it meets the orbital floor. However, the actual measurement varies dramatically, as does the deformity, in individual patients. Secondly, the attachment sweeps anteriorly as it goes from medial to lateral, but again the amount is variable. This information is useful when planning each surgery, as some individuals have a full crescent deformity, or “deep circle”, extending laterally all the way around the lid – cheek junction. Thirdly, the distance of the orbital septal attachment posteriorly from the infraorbital rim differs between males and females. In performing an arcus marginalis release, it should be noted that the inferior oblique muscle has previously been found to originate 5.14 mm +/-1.21 posterior to the central infraorbital rim. Hence, special care should be taken in the central release of the arcus marginalis in male patients, as not to injure the inferior oblique muscle. Our surgical approach has centered around individualizing each surgical procedure to address the specific anatomic deformity. We have been able to perform this arcus marginalis and fat repositioning primarily through a transconjunctival approach using internal suture fixation (Figure 2a,b 3a,b demonstrate tear trough/crescent deformity; 2 c,d 3 c,d represent postoperative result via transconjunctival arcus marginalis approach).
View Synopsis (.doc format, 427.0 kb)
See more of Cosmetic
Back to Plastic Surgery 2003 Complete Scientific Program
Back to Plastic Surgery 2003 Meeting home