Wednesday, October 29, 2003 - 8:00 AM
3232
A Computer-Based Surgical Simulator for Cleft Lip Planning and Repair
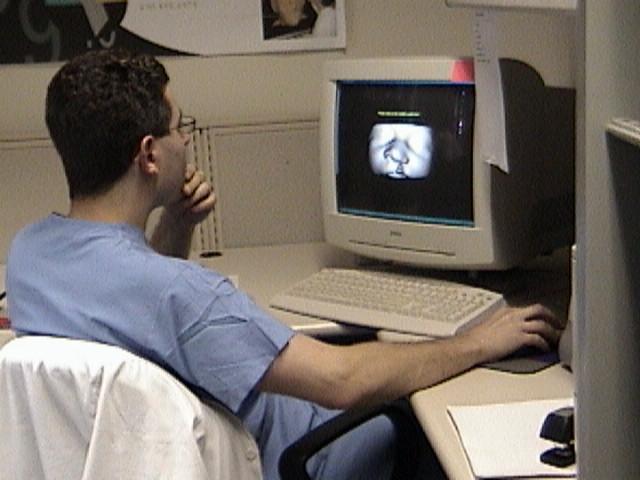
The objective of this project was to develop a computer-based surgical simulation system for cleft lip planning and repair. This system allows the user to interact with a virtual patient to perform the traditional steps of cleft-lip repair. The system interfaces to force-feedback (haptic) devices to track the user's motion and provide feedback during the procedure, while performing real-time soft-tissue simulation.
An eleven-day old unilateral cleft-lip and palate patient was previously CT scanned for ancillary diagnostic purposes using standard imaging protocols and 1mm slices. High-resolution 3D meshes were automatically generated from this data using the ROVE software created in our lab. The resulting 3D meshes of bone and soft-tissue were instilled with physical properties of soft tissues for purposes of simulation. Once these preprocessing steps were completed, the patient's bone and soft-tissue data are presented on the computer screen in stereo and the user can freely view, rotate, and otherwise interact with the patient's data in real-time. The user is prompted to select anatomical landmarks on the patient data for preoperative planning purposes, then their locations are compared against that of a “gold standard” and a score, derived from their deviation from that standard and time required, is generated.
The user can then move a haptic stylus and guide the motion of the virtual cutting tool. The soft tissues can thus be incised using this virtual cutting tool, moved using virtual forceps, and fused in order to perform any of the major procedures for cleft-lip repair. Real-time soft tissue deformation of the mesh realistically simulates normal tissues and haptic-rate (>1kHz) force-feedback is provided. The surgical result of the procedure can then be immediately visualized and the entire training process can be repeated at will.
A short evaluation study was also performed. Three groups (nonmedical, plastic surgery residents, and attending physicians) of six-people each performed the anatomical marking task of the simulator four times. Results showed that the plastic surgery residents scored consistently better than the people without medical background and even better than attendings. Every person's score increased with practice, and the length of time needed to complete the eleven markings decreased. The data was compiled and showed which specific markers consistently took users the longest to identify as well as which locations were hardest to accurately mark.
Our findings suggest that the simulator is a valuable training tool, giving residents a way to practice anatomical identification for cleft lip surgery without the risks associated with training on a live patient. Educators can also use the simulator to examine which markers are consistently problematic, and modify their training to address these needs.
See more of Technology Based Procedures and Advancements
Back to Plastic Surgery 2003 Complete Scientific Program
Back to Plastic Surgery 2003 Meeting home